MDRF, U.S. researchers demand precise treatment after discovering new monogenic diabetes subtype
Dr. V. Mohan, Chairman of the Madras Diabetes Research Foundation and Dr. Radha Venkatesan, Director of Genomics at Madras Diabetes Research Foundation at the press conference | Photo source: Hindu
Scientists at the MADRAS Diabetes Research Foundation (MDRF) in Chennai, in collaboration with the Washington University School of Medicine in St. Louis, USA, have discovered subtypes (Mody) of mature diabetes in previously unaccepted young people (Mody) and called for a wider range of diabetes and precision treatments for diabetes, especially those with diabetes in India.
The findings were made to the media at a meeting held at the MDRF on Thursday.
Mody is a rare, hereditary form of diabetes caused by mutations in a single gene that usually occurs in adolescents and young people. Doctors say that although 13 Mody subtypes have been confirmed so far, the newly identified longer challenges to this situation.
Genetic testing is required in diabetes management
The breakthrough not only increases scientific understanding, but also highlights the urgent need to incorporate genetic testing into routine diabetes care, the researchers said. They noted that this could mark a turning point in improving diagnosis, treatment and long-term disease management in thousands of people with single-gene diabetes forms or misclassified forms.
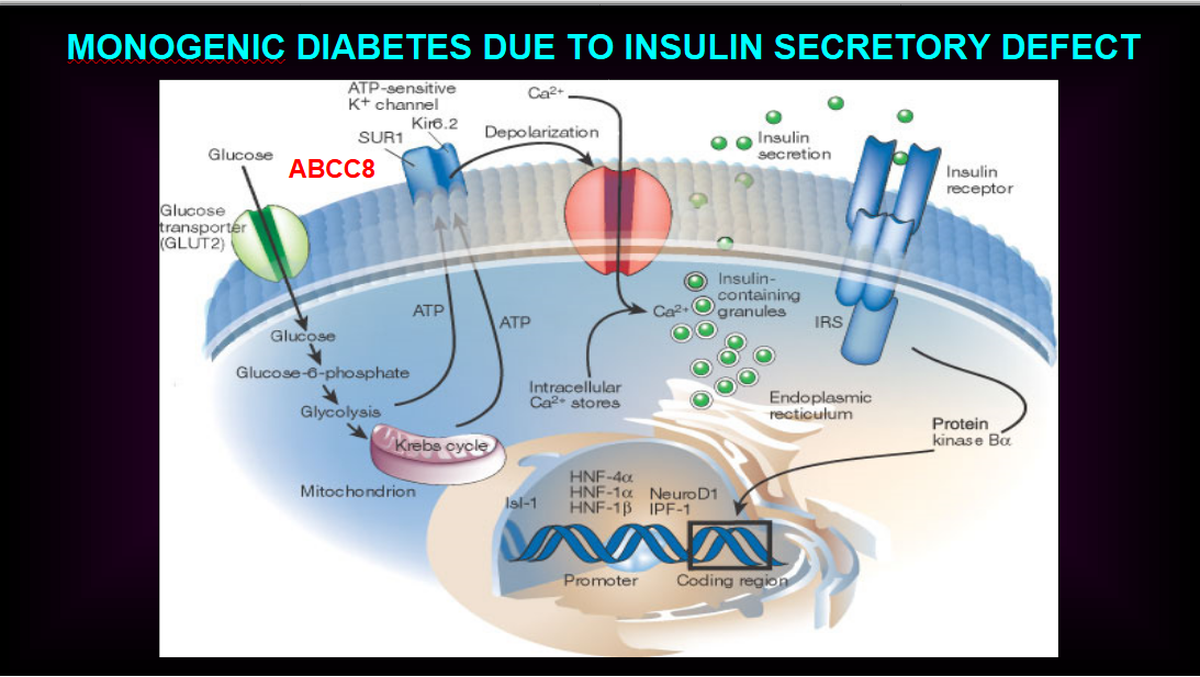
These defects mainly affect the pancreatic beta cells responsible for insulin synthesis and secretion. |Picture source: Special arrangement
Research, Published in journals – diabetes –Identification of diabetes-associated associations in the United States recognizes loss of function (LOF) mutations in the ABCC8 gene (which helps regulate insulin release in pancreatic islets by controlling channels that respond to glucose levels and allows insulin release into the bloodstream when needed), in contrast, when needed (GOF) link (GOF) mutations (GOF) mutations are opposite to the Internet of Mody and neosal and Neesal. The novel variants lead to early blood sugar hypoglycemia, followed by late onset diabetes, a progress previously undocumented in Mody cases.
Colin G. Nichols, principal investigator at the University of Washington School of Medicine, emphasized in the study that LOF mutations damage potassium channel function in pancreatic beta cells, thus disrupting insulin secretion. He said the study marked the first time that it has been observed to go from congenital hyperinsulin to diabetes in mature diabetes in young environments.

Clinical significance and therapeutic possibilities
Radha Venkatesan, executive science officer at MDRF Molecular Genomics and co-leader author, highlighted the clinical significance of this finding. “This variant does not respond to conventional treatments, such as sulfofuruli, which are effective in other Mody forms. Understanding the underlying genetic mechanisms is key to guiding appropriate treatments,” she said.
Insulin secretion is the process by which pancreatic beta cells release insulin into the blood. |Picture source: Special arrangement
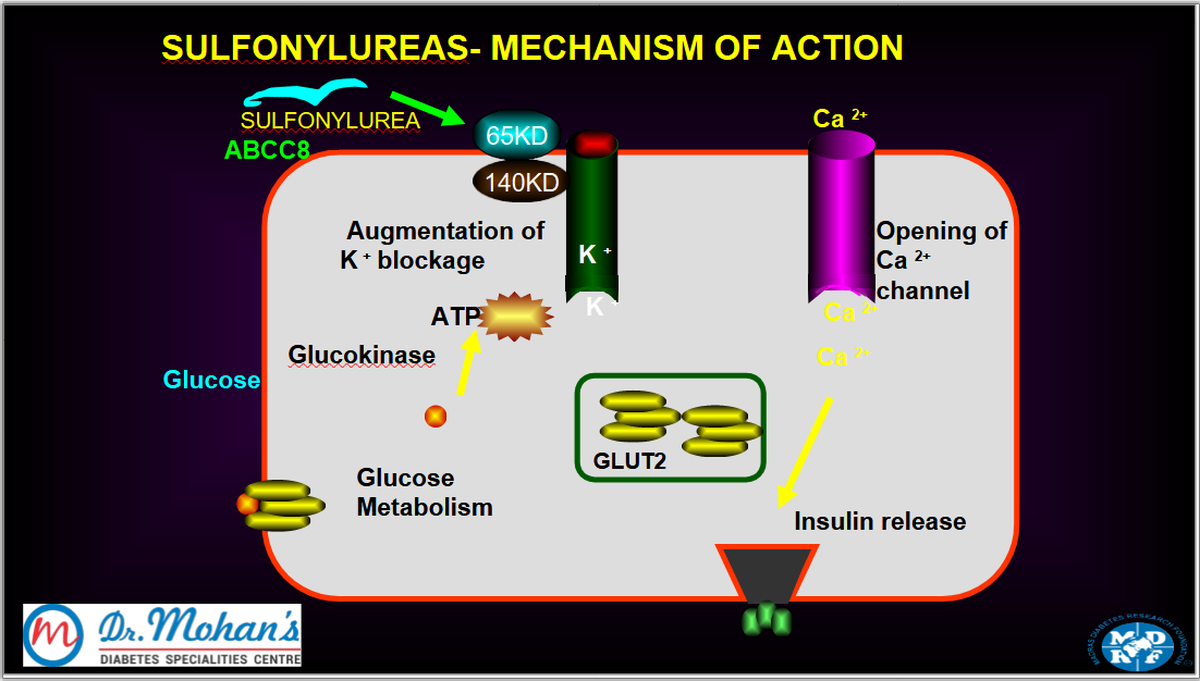
Lower blood sugar levels by stimulating the release of insulin from the pancreas | Image source: Special arrangement
MDRF Chairman V. Mohan reiterated the importance of incorporating genetic testing into standard diabetes diagnosis. “Many Mody patients are still not diagnosed or misclassified as having type 1 or type 2 diabetes. This finding enhances cases of precise diagnosis and treatment,” he said.
These findings are based on clinical data and laboratory analyses of Indian patients. The researchers believe that expanding access to genetic testing may lead to early detection and more effective care in people with a single-gene form of diabetes.
publishing – May 8, 2025 at 09:54 pm ist



